BACKGROUND:
It is estimated that 8480 persons in USA will be diagnosed with Hodgkin Lymphoma (HL) in 2020 accounting to approximately 0.5% of all new cancer diagnoses. The advent of new treatment options has improved the outcomes of this disease and 5-year relative survival rate is 87.4% currently. However, studies have shown that outcomes of HL have been worse in Hispanics (Annals of Oncology, PMID: 22241896) especially in late stage disease and HI experience up to a 35% higher risk of HL specific mortality than whites (AACR,PMID: 26826029). There is an unmet need in the field and dossiers on underrepresented ethnic minorities need to be carefully considered, compared to existing data. Our study aims to compare survival outcomes in Hispanics (HI) vs Non-Hispanics (NH) with HL and to our knowledge this is the largest cohort of patients from an area that represents a large proportion of HI population in the USA.
METHODS:
This is a retrospective study that examines HL patients obtained from Texas Cancer Registry (TCR) database between 2006-2016 and identified by the International Classification of Diseases for Oncology Third Edition (ICD-O-3) code list. All patient data was provided to us de-identified. Standard demographic variables collected include gender, race, ethnicity, dates at diagnosis and death, primary payer at diagnosis, subtype of lymphoma, stage, treatment modality, poverty index among others. Categorical outcomes were summarized with frequencies and percentages while age (years), the only continuously distributed outcome was summarized with the mean and standard deviation. The significance of variation in the distribution of categorical outcomes with ethnicity (HI vs NH) was assessed with Fisher's Exact tests or Pearson's Chi-square tests as appropriate; age was assessed with T-tests or Wilcoxon tests as appropriate. Survival time (years) was measured from date of primary diagnosis to death. Patients not coded as dead were considered censored on survival time at the date last seen. Survival distributions were described with Kaplan-Meier curves and significance of variation in median survival with ethnicity was assessed with log rank testing. At risk tables were computed based on the Kaplan-Meier estimate of the survival curve. All statistical testing was two-sided with a significance level of 5%. Corrections for multiple testing were not applied. The R language [R Core Team (2013). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria] was used throughout.
RESULTS:
We identified 6353 patients with HL, of which 1843 were HI (29%), 4510 NH (71%). Median age of diagnosis in HI was 41.3 vs 42.3 in NH (p = 0.084). Males were more frequently affected, 56.5% in HI vs 54.8 in NH (p = 0.213). Most frequent poverty index bracket for HI was between 20-100% vs 10-19.9% for NH (p < 0.001). Most frequent payment model amongst both groups was private insurance with 28.1% in HI vs 45.1% in NH (p < 0.001). Metro/non-border most frequent locality amongst both groups (p value n/a) with Harris county accounting to 15.7% of HL in HI vs 16.5% of HL in NH. Bexar county accounted for 12.5% of HL in HI vs 5.2% of HL in NH. Most common stage at diagnosis in both groups was III/IV with 43% in HI vs 33.7% in NH (p < 0.001). In both groups most frequent chemotherapy included multiple agents, 57.1% in HI vs 48.8% in NH (p < 0.001). Majority in both groups neither got any radiation, 77% in HI vs 76.5% in NH (p = 0.208) nor hematologic transplant, 92% in HI vs 88.6% in NH (p = 0.01).
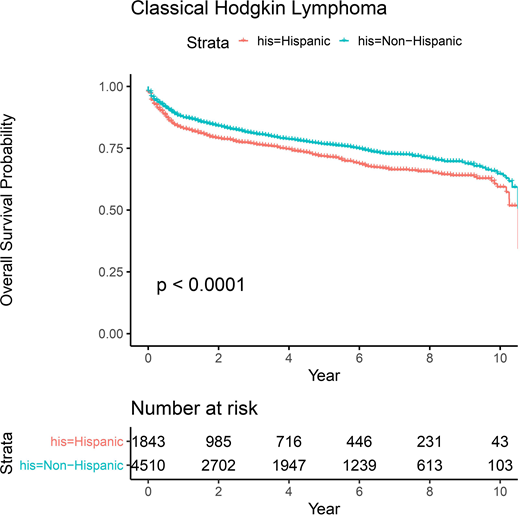
We found the median overall survival time in HI was 10.5 years vs 10.8 years in NH; the overall survival probability for HI vs NH at 2 years was 0.8 [CI 0.771-0.811] vs 0.85 [CI 0.83-0.853], at 5 years was 0.72 [CI 0.694-0.743] vs 0.77 [CI 0.753-0.782] and at 10 years was 0.60 [CI 0.544-0.646] vs 0.65 [CI 0.615-0.679].
CONCLUSION:
Our study demonstrates that amongst the population of Texas, HI patients with HL have a statistically significant worse overall survival probability (p value < 0.0001) when compared to NH patients with HL. It is of paramount importance that outcomes for all racial and ethnic groups continue to improve but very little is known about the basis for these differences. This warrants a deeper investigation into the biological and non-biological determinants for these differences.
Diaz Duque:ADCT Therapeutics: Research Funding; Molecular Templates: Research Funding; AstraZeneca: Research Funding; Hutchinson Pharmaceuticals: Research Funding; Seattle Genetics: Speakers Bureau; Verastem: Speakers Bureau; AbbVie: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal